Johnson Mathers Nursing Home | Kentucky Nursing Home Abuse and Neglect Attorneys
The decision to place a loved one in a nursing home is not one that is taken lightly. You take the time to visit the selected home and meet the doctors and nurses that will be caring for your loved one. But what happens if you have put your faith in the wrong facility?
ABOUT JOHNSON MATHERS NURSING HOME
Johnson Mathers Nursing Home is located in Nicholas County, KY, and is a Medicare/Medicaid participating long-term care facility. It is a “for-profit” center and has a 104-bed capacity. They offer a host of services in addition to 24-hour nursing care. Some of their services include:
- Social Services
- Registered Dietitian Services
- Respite Care
- Post-Surgical Care
- Respiratory Care
- Pain Management
- Cardiac and Stroke Care Rehabilitation
- Hospice Services
- Acute Care Services
- Physical, Speech, and Occupational Therapy
Johnson Mathers Nursing Home has a history of poor regulatory compliance. A 2021 survey from the Cabinet for Health and Family Services reveals the depth and breadth of their violations in a 414-page report. Some of the serious deficiencies, violations, and safety concerns at Johnson Mathers Nursing Home include:
- “…the facility failed to ensure each resident was treated with respect and dignity and care provided in a manner and in an environment that promoted maintenance or enhancement of his or her quality of life, recognizing each resident’s individuality.” (ID F 550, pg. 6)
- “…the facility failed to have an effective system in place to limit charges on residents’ personal funds. In addition, the facility failed to protect residents’ personal funds from unnecessary purchasing of items for residents using Stimulus money and for any item not required to achieve the goals stated in the residents’ care plans.” (ID F 571, pg. 15)
- “…the facility failed to ensure residents were free from misappropriation of property (narcotic pain medication).” (ID F 602, pg. 74)
- “…the facility failed to initiate a timely and thorough investigation in order to prevent and protect residents from further misappropriation of property (controlled medications), after residents made allegations of not receiving medications and that staff were taking the medications for fifteen (15) of forty-four (44) sampled residents.” (ID F 610, pg. 131)
- “Based on observation, interview, record review, and review of the Centers for Medicare and Medicaid Services (CMS), “Resident Assessment Instrument (RAI) Manual 3.0”, it was determined the facility failed to develop and/or implement a person centered Comprehensive Care Plan (CCP) for each resident that included measurable objectives and timeframes to meet a resident’s medical, nursing, and mental and psychosocial needs that were identified in the comprehensive assessment.” (ID F 656, pg. 184)
- Based on interview, record review, review of the Emergency Medical Services (EMS) Run Sheet, American Heart Association Cardiopulmonary Resuscitation (CPR) guidelines, and the facility’s policy, it was determined the facility failed to ensure licensed nursing staff met professional standards of practice in providing CPR.” (ID F 658, pg. 214)
- The facility failed to ensure a resident with limited mobility received appropriate services, equipment, and assistance to maintain or improve mobility with the maximum practicable independence, unless a reduction in mobility was demonstrably unavoidable.
- “…the facility failed to ensure each resident’s environment was free from accident hazards over which the facility had control; and failed to provide supervision and assistive devices to each resident to prevent avoidable accidents.” (ID F 689, pg. 261)
- “…the facility failed to maintain a system to ensure controlled medications received from the pharmacy were accounted for; with only one (1) nurse required to sign for incoming controlled substances. In addition, the facility failed to have an effective system in place for reconciliation of each controlled narcotic medication, and there was no documented evidence that causes of the discrepancies were thoroughly investigated.” (ID F 755, pg. 288)
- “…the facility failed to meet current requirements for a qualified Dietary Manager. The current Dietary Manager (DM) was not certified or currently enrolled in a Certified Dietary Manager (CDM) course, as to meet the requirements to be certified within one (1) year after hire. In addition, the Consultant Registered Dietitian (RD) was not available to provide proper supervision/consultations for the Dietary Manager.” (ID F 801, pg. 344).
- “…the facility failed to store, prepare, and distribute food under sanitary conditions and in accordance with professional standards for food safety.” (ID F 812, pg. 349)
- “…the facility failed to be administered in a manner that enabled effective use of its resources to attain and maintain the highest practicable physical, mental, and psychosocial well-being for residents.” (ID F 835, pg. 356)
- “…the facility failed to have an effective governing body that was responsible for establishing and implementing policies regarding the management and operation of the facility.” (ID F 837, pg. 376)
- “…the facility failed to establish and maintain an infection prevention and control program designed to provide a safe, sanitary and comfortable environment and to help prevent and control the development and transmission of communicable diseases and to implement interventions per the Centers for Medicare and Medicaid Services (CMS), the Centers for Disease Control and Prevention (CDC), and the Kentucky Department for Public Health (Health Department) state guidelines for COVID-19.” (ID F 880, pg. 397)
- “…the facility failed to maintain discharge from exits in accordance with National Fire Protection Association (NFPA) standards.” (ID K 271, pg. 410)
- “…the facility failed to meet the requirements for Protection of Hazards, in accordance with the National Fire Protection Agency (NFPA) standards.” (ID K 271, pg. 410)
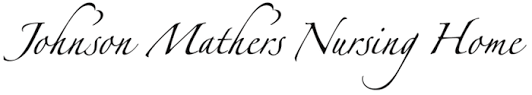
Johnson Mathers Nursing Home has consistently received mid to low ratings on Medicare with below-average in inspections and staffing. As of February 2022, Johnson Mathers Nursing Home is no longer eligible for The Centers for Medicare and Medicaid funding. Medicaid is the single largest funding source for nursing homes across the nation.
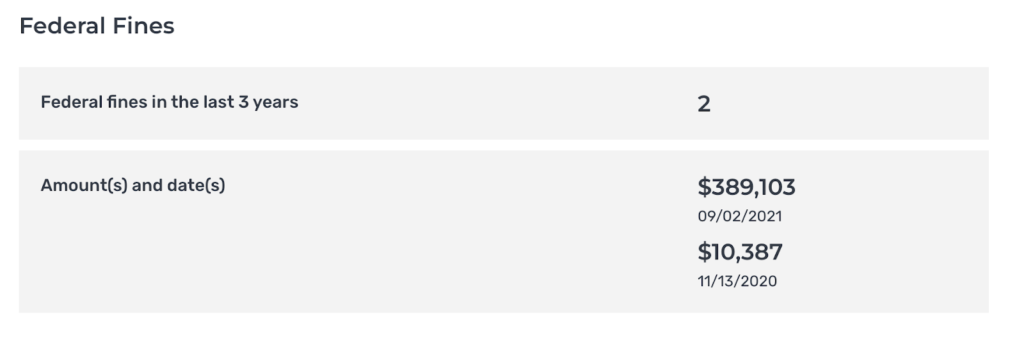
Johnson Mathers has seen two federal fines in the last 3 years, totaling $399,490.
As of February 2022, Johnson Mathers Nursing Home is no longer eligible for The Centers for Medicare and Medicaid funding. Medicaid is the single largest funding source for nursing homes across the nation.
SOURCES
If you have or had a loved one that is a resident of Johnson Mathers Nursing Home, and you suspect they have been mistreated, contact our experienced lawyers today.
Our Kentucky nursing home abuse lawyers have passionately advocated for thousands of clients in several states, uncovering the secrets, analyzing the facts, and helping residents and their families pursue justice. With Circeo Law Firm, our clients can trust that responsible parties in the abuse will be held accountable, and victims will receive the compensation they deserve. If you or a loved one has suffered from negligence or abuse at a nursing home or assisted living facility, contact us for a free consultation.
DISCLAIMER
The Kentucky Cabinet compiled the results of the survey mentioned above for Health and Human Services and the Department of Health and Human Services. The complete list of reports can be found here.
The referenced survey was conducted on September 2, 2021, by the Department of Health and Human Services Centers for Medicare & Medicaid Services, identification number 185028. The complete 414-page survey can be found here. Johnson Mathers Nursing Home is required to submit a plan of correction in response to a statement of deficiencies. If the findings or deficiencies have been corrected, a statement that the finding or deficiencies have been corrected has been released.
This blog is not authorized or endorsed by the Cabinet for Health and Family Services, Office of the Inspector General, the Centers for Medicare and Medicaid Services, or any other government agency.